If you have been following me recently will know that I am working through my digestion and energy challenges following my recent stool test.
I was relieved when my gluten antibodies (anti-gliadin IgA) came back negative but one thing I didn’t want to have to do was give up FODMAPS for two main reasons:
- I love onions and garlic

- It’s a pain
FODMAP stands for Fructose, Oligosaccharide, Disaccharide, Monoamines and Polyols. It’s a bit of a mouthful so I am sure you can see why these are summarised as FODMAPS.
Ultimately these are types of carbohydrates which are more susceptible for fermentation in the upper GI tract, which, when overgrown with bacteria, can lead to symptoms like bloating, cramping, diarrhoea, constipation and symptoms of IBS.
Despite my supplement regime, I was still experiencing a lot of stomach bloating. It seemed to be even worse than before.
I eat a lot of onions, garlic, legumes and broccoli. In fact, I was eating raw broccoli scrunched up in a salad with lot’s of avocado (which can also be a FODMAP). So the pain of staying the same eventually got greater than the pain of embarking on my new low FODMAP lifestyle and I took the plunge.
I have several clients who follow a low FODMAP diet and it is becoming increasingly common as I start to work with more and more clients on their digestion alongside their weight loss, that I am asking them to remove FODMAPS.
I therefore thought it would be helpful for me to write how I approached it and what I’ve been eating this past week, to make life a little easier for those who are embarking on a Low FODMAP plan.
The first thing I have to say is that FODMAPs can be confusing. Different resources will tell you different things. I decided to commit to one resource and then let my body feedback the rest.
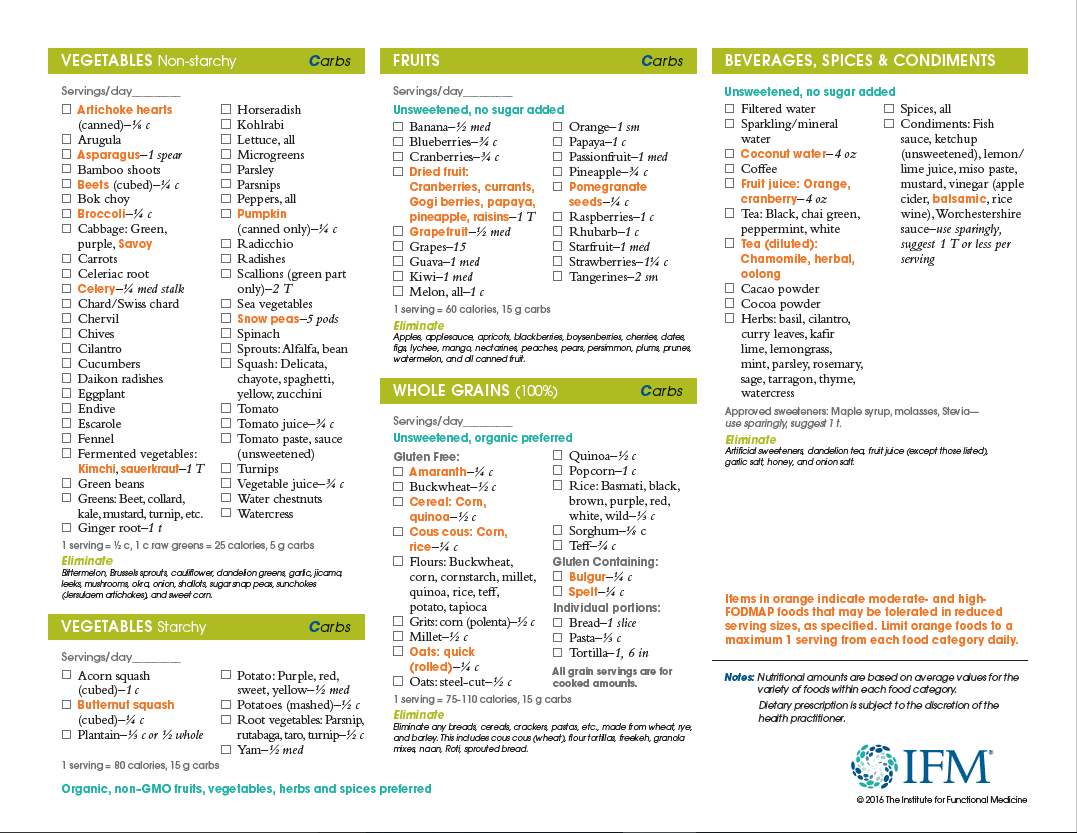
I used the IFM Low FODMAP food plan.

The way I approached it was as follows:
- I went through the food plan and write down a list of everything I could eat based on the foods I frequently buy and was already eating
- I then went through a list of the foods highlighted in orange and wrote down any I was already eating and noted the portion size I should limit myself to if I was going to still include it.
- Most of “orange foods” I was happy to exclude but I still wanted to include some quinoa, sesame and sunflower seeds (for my seed cycling regime), avocado and I had already had some hummus and beans in the cupboard that I needed to use.
- I then photographed the list to keep on my phone so if I find myself at the supermarket or at a restaurant I can double check what I should buy or what I need to avoid.
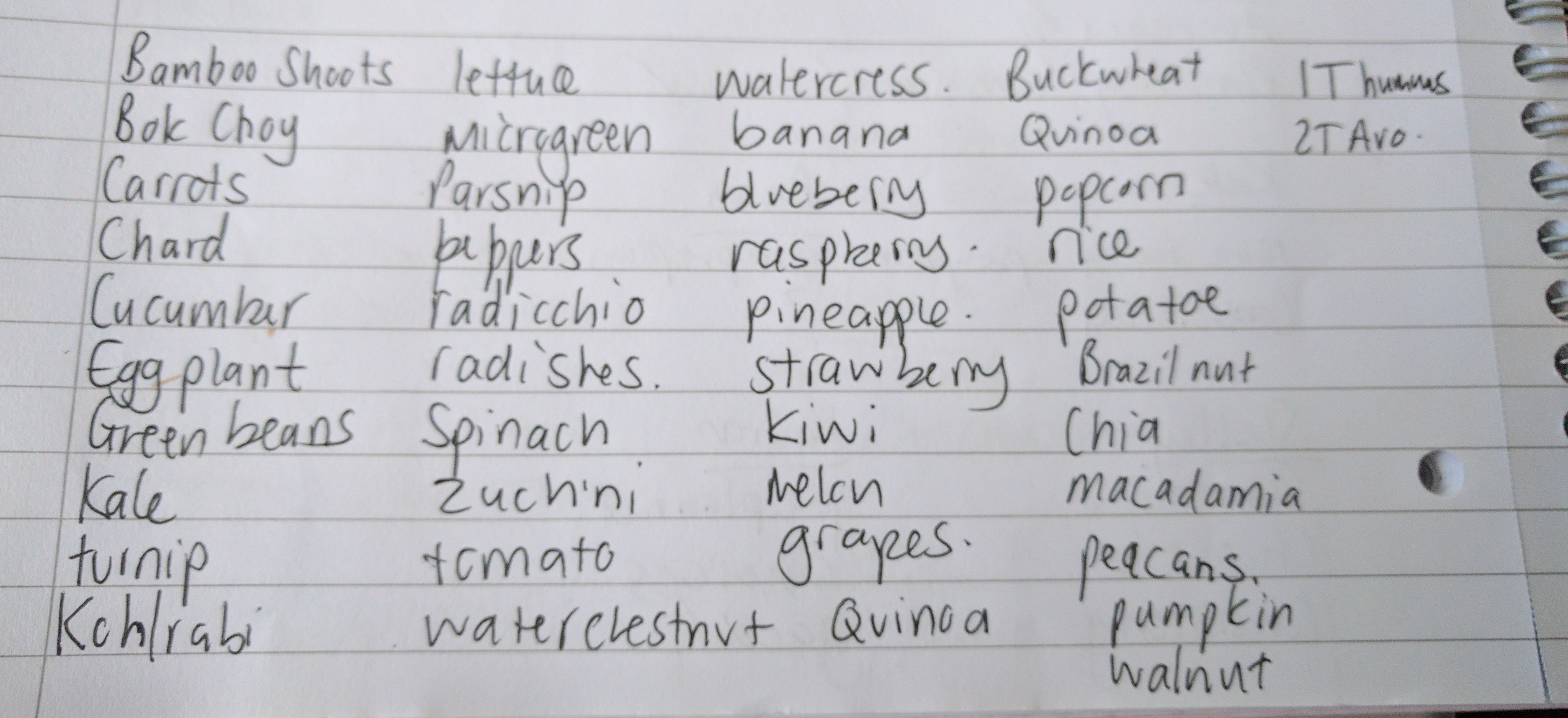
This was my list before I added dairy; feta, haloumi and parmesan
I kept things simple.
I can be a creature of habit when it comes to food. So when I share my food diary, you will probably notice a lot of the same things repeating. I tend to eat a lot of the same and then get a bee in my bonnet about something new and eat a lot of that for a bit.
What I mostly tried to do is work with recipes I was already using and adapt them or just eat simple foods and make them tasty with lots of olive oil and lemon juice.
Although garlic and onion are to be excluded on a Low FODMAP diet a bought a garlic and onion salt to add flavour to dishes, which so far, I seem to be getting away with in small amounts. I don’t have any idea how these compare to normal onions and garlic so it might not mean that anyone following a low FODMAP diet would get away with them. As an alternative, you can infuse olive oil with garlic or add large chunks of onion to a dish and remove them after flavouring the oil.

Day 1

Breakfast
1 left over gluten free pork sausage, 2 eggs and 100g egg white. Spinach and Kale with olive oil, lemon juice and sumac
Lunch
Watercress, spinach and 1 tin of tuna in olive oil, 2 carrots and 2 tbsp hummus and left over black bean spaghetti
Dinner
Pan-fried Salmon, with courgetti sautéed in olive oil and parmesan
Day 2

Breakfast
You’ll see my breakfast smoothie feature a lot. I love it! I have it after working out most mornings and I feel like I have perfected the recipe to get a great consistency. It is as follows:
- 1 banana
- 120-150g frozen raspberries
- 5 ice cubes
- 10g-15g maca powder
- 150ml-200ml almond milk (I use the alpro almond milk which is slightly sweet)
- 5g Ashwaganda Powder (I take this to support my adrenal glands, it is also good for the immune system and mitochondria)
- 10g L-glutamine (great for healing the cells of the gut lining and also for the immune system)
- 30g beef protein (I’m using this at the moment because I think I was reacting to whey)
- 1 tbsp chia seeds
- 1 tbsp sunflower seeds or 1 tbsp flax and 1 tbsp pumpkin seeds depending on where I am in my cycle.
A malteser bunny (yep, it’s low FODMAP! A friend of mine was advised it was okay to eat maltesers on a Low FODMAP diet by an NHS dietican), not in the smoothie though, I had this later as a snack!

Lunch
Watercress, spinach, quinoa and 1 tin of tuna in olive oil, 2 carrots and 2 tbsp hummus and left over black bean spaghetti
Dinner
Cod with sundried, anchovies, tomatoes, basil, lemon juice, parmesan, black venus rice, courgetti and olives pan-fried in olive oil
Day 3

Breakfast
2 boiled eggs, 1 gluten free crumpet, 2 slices of panfried haloumi and a tbsp. avocado
Lunch
Protein pancakes: banana, chia, 20g oats, beef protein, cinnamon, cooked in coconut oil serves with raspberries, olive oil and chopped dark chocolate coated brazil nuts
Dinner
Thai takeaway – red curry with chicken and all the vegetables were low FODMAP
Day 4
Breakfast
Gluten free chicken sausages, 2 boiled eggs and greens with olive oil and lemon juice
Lunch
Popcorn at the cinema – it was a Sunday 
Dinner
Pan-fried steak in olive oil with spinach, mushrooms, creams, black rice
Day 5
Breakfast
Protein smoothie & 2 squares of 90% dark chocolate and 1 tbsp tahini
Lunch
Watercress, spinach, 50g black rice and 1 tin of tuna, 1 tbsp olive oil. lemon juice, sumac and 30g of haloumi
1/2 red pepper and 1 tbsp hummus
Dinner
Mince cooked in coconut oil, cajun spice, smoked paprika and tinned tomatoes. I had great intentions of bulking it out with carrots, celery, mushrooms and courgette before I realised I had finished them off so I added in 50g of cold quinoa instead. It was simple, yet delicious with the spices and you can always add more greens or courgetti
Day 6
On day 6 I had the same smoothie, but, because I had been running that morning I felt incredibly hungry so went in for a second breakfast of gluten free crumpets, butter, marmite, a sprinkling of parmesan and 2 boiled eggs. This is my favourite treat breakfast!

Then at lunch time I was back on the tuna salads just using up bits left in the fridge however, I managed to take a photograph this time, yet in doing so, completely forgot to scrunch up my green leaves in the olive oil and lemon juice. This time I added some romaine lettuce instead of spinach and finished off the last of the kale and watercress.
Although this salad looks pretty sparce, the following Low FODMAP items could have been used to make it more colourful and filling:
- grated carrot
- cucumber
- micro-greens
- peppers
- radishes
- tomatoes
- 2T of Avocado
- Nuts and seeds such as pumpkin, walnuts, pecans, brazils or macadamia nuts (always quite nice if you toast them first before throwing into a salad)
- A little feta or hard cheese
- I sometimes also like sliced grapes or blueberries in a salad, these are also low FODMAP options

Dinner
For dinner that night I had the same cod dish again. But this time I managed to photograph it. It’s so easy to do, you just blitz up some sundried tomatoes, parmesan, lemon juice, basil, a couple of anchovies and sumac, smear it on the cod and bake for about 20 minutes at 200 degrees

This was served with some vegetables with I essentially just stir fried up in olive oil…

Day 7
The final day was smoothie again plus 2 pieces of 90% dark chocolate and 2 sliced of haloumi cheese (bit random but that was it)
For lunch I had left over cod with a side salad of romaine lettuce, olive oil, quinoa, my 2 tbsp allowance of avocado and some red pepper slices…. oh and another Malteser bunny 

Dinner
Finally dinner was a beef dish I had made in the slow cooker the previous day using the following:
2 tbsp olive oil
2 tbsp cajun spice
2 tbsp smoked paprika
1kg diced organic stewing steak
2 tins of chopped tomatoes
400g carrots, chopped
5 celery stalks, chopped
I basically just browned the steak in a pan with olive oil and spices and then threw it all in the slow cooker for 8 hours (you could even do this overnight).
Day 8
As I didn’t go to the gym today, I had a lower carb breakfast of heck chicken sausages, scrambled eggs and egg white, final bits of salad left in the fridge (food delivery comes today) and I later treated myself to an Om Bar chocolate from the health food shop when I went to my ceramics lesson.
Lunch was another tuna salad with freshly delivered greens (watercress, lambs lettuce, spinach and broccoli sprouts), carrots, hummus, tuna, olive oil and lemon juice.
The day was finished off with left overs from the slow cooked beef recipe the day before.


And that brings me to the end of my week (+one day) following a low FODMAP diet.
I must say, I had perhaps suspected it was something I may benefit from for a while. But I wasn’t prepared to full commit to it because, ultimately, it meant the effort of changing my routine.
I am amazing at how easy it became even after a few days because I put a little effort in at the beginning to work out what I needed to do and get organised.
Finally, I would also say, my digestion has calmed down massively over the past week and it’s lovely not to go to bed in the evening with a slightly distended belly.

I run a small Online Women’s Weight Loss Program that offer a personalised nutrition and exercise support to produce life changing and life-lasting results.
If you want to give up the guessing game and have someone just tell you what to do and hold you accountable to actually doing it then this is probably exactly what you have been waiting for.
Life doesn’t get better by chance, it gets better by choice. Now you have a moment where you can choose to take a step towards a very different future and join the community of like minded women who are not just losing weight, but transforming their lives, filling them with happiness and health.
To find out more about how my coaching program can help you, please fill out the application below to book a complimentary breakthrough call and find out out about working with me in more detail.